How to Help Someone with OCD: A Guide for Supporters (Includes a Free OCD Test)
November 11, 2025 | By Samuel Griffin
When someone you care about is battling Obsessive-Compulsive Disorder (OCD), it's tough to know how to help. You want to offer solid support without accidentally making things worse. This guide offers compassionate, practical ways to understand OCD and become a truly effective ally on their path to recovery. For those seeking a gentle starting point, a confidential screening tool can offer valuable initial insights.
Understanding OCD: The First Step Towards Effective Support
Before you can offer meaningful help, it’s crucial to understand what your loved one is truly experiencing. OCD is more than just being neat or double-checking things; it's a complex and often debilitating mental health condition. Grasping the fundamentals is the first step in providing genuine, empathetic support.
What Exactly is Obsessive-Compulsive Disorder?
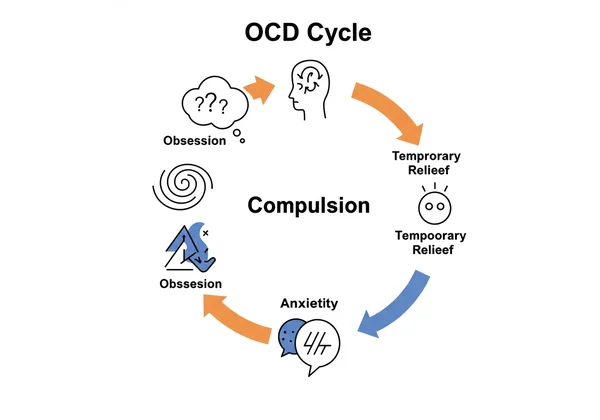
Think of OCD as a relentless cycle where intrusive thoughts (obsessions) lead to repetitive actions (compulsions). What is OCD, really? Obsessions are intrusive, unwanted, and persistent thoughts, images, or urges that cause significant anxiety and distress. Compulsions are repetitive behaviors or mental acts that the individual feels driven to perform in response to an obsession. The compulsion is a desperate attempt to neutralize the anxiety or prevent a feared outcome, but the relief is only temporary, and the cycle continues.
Common Signs and Symptoms to Recognize
Recognizing the signs of OCD is key to understanding the need for support. While symptoms vary widely, some common OCD symptoms include:
- Obsessions: Fear of contamination, doubts about having locked the door or turned off the stove, unwanted aggressive or horrific thoughts, or a need for things to be in a perfect, symmetrical order.
- Compulsions: Excessive hand washing, repetitive checking, ordering and arranging things in a precise way, compulsive counting, or silently repeating words or prayers. It's important to remember that these are just examples. OCD can manifest in countless ways, many of which are not visible to others (a subtype often called Pure O).
The Impact of OCD on Daily Life and Relationships
The constant battle with intrusive thoughts and time-consuming compulsions can be exhausting. The impact on daily life is often profound, affecting work, school, and social activities. For families and partners, OCD can create tension and confusion. You might feel frustrated by behaviors you don't understand or find yourself drawn into rituals, which can strain even the strongest relationships. Understanding this impact fosters the patience and empathy needed to be a true ally.
Practical Ways to Offer Compassionate Help
Once you have a foundational understanding, you can begin offering practical and compassionate support. Your role is not to be a therapist but to create a supportive environment that encourages recovery. Even seemingly small, consistent efforts from you can profoundly impact their journey.
Effective Communication Strategies
Open, non-judgmental dialogue is essential. When communication with someone with OCD, listen to their experience without minimizing their fears. Instead of saying, "Don't worry about it," try, "I can see how distressing that thought is for you. I'm here for you." Validate their feelings, not the obsession itself. This shows you care about their emotional state while not reinforcing the OCD's logic.
Setting Healthy Boundaries and Reducing Accommodation
This is one of the most challenging yet crucial aspects of helping. "Accommodation" is when you participate in your loved one's compulsions—like repeatedly providing reassurance or checking things for them. While it feels helpful in the moment, it strengthens the OCD cycle. Setting boundaries for OCD means gently refusing to accommodate these rituals. You can say, "I love you and I want to support you, but I know that giving you reassurance isn't helpful in the long run. We can sit together through this anxiety."

Empowering Them Towards Self-Care and Managing Stress
Stress is a significant trigger for OCD symptoms. Encourage healthy coping mechanisms and self-care practices. Suggest activities you can do together, like going for a walk, practicing mindfulness, or engaging in a hobby they enjoy. Managing stress with OCD is a vital skill, and your support can make it feel more achievable. Helping them find healthy outlets can reduce the overall intensity of their symptoms and empower them to regain control.
What NOT to Do or Say: Avoiding Common Pitfalls
Knowing what to avoid is just as important as knowing what to do. Well-intentioned comments can sometimes be hurtful or counterproductive. Understanding these pitfalls is a key part of learning what not to say to someone with OCD.
Why Reassurance-Seeking Can Worsen OCD
The urge for certainty is a core feature of OCD. Your loved one might repeatedly ask questions like, "Are you sure I'm not a bad person?" or "Are you sure the door is locked?" While your instinct is to soothe them, providing that comfort feeds the disorder. Reassurance seeking in OCD creates a dependency, teaching the brain that the only way to cope with anxiety is through external validation. Resisting this can be difficult but is vital for their recovery.
Minimizing Feelings or Saying "Just Stop"
Phrases like "Just stop thinking about it," "It's all in your head," or "You're being irrational" are deeply invalidating. A person with OCD is often acutely aware that their fears are irrational, but they cannot simply will them away. Remember to avoid these phrases to avoid with OCD, as they can increase feelings of shame and isolation.
Blaming or Shaming: The Dangers of Stigma
Never blame your loved one for their symptoms or express frustration in a way that shames them. OCD is a neurobiological disorder, not a character flaw or a choice. Battling OCD stigma begins at home. Your acceptance and unconditional support create a safe space where they feel comfortable opening up and seeking the help they need.
Navigating Your Relationship When OCD is Present
OCD doesn't just affect the individual; it impacts the entire family system. Learning to navigate your specific relationship dynamic is crucial for maintaining healthy connections while supporting recovery, an important aspect of dealing with OCD in relationships.
Supporting Your Partner with OCD
When your partner has OCD, it can feel like the disorder is a third person in your relationship. Work together as a team against the OCD. Celebrate small victories, be patient during setbacks, and ensure you continue to nurture the parts of your relationship that are separate from the disorder. Consider suggesting you both learn more by taking a preliminary online test together to better understand the symptoms.
Guiding Your Child or Teen Through OCD Challenges
For parents, watching your child with OCD can be heartbreaking. The key is to balance empathy with firm, loving boundaries. Work closely with a therapist who specializes in pediatric OCD to learn how to parent effectively without accommodating rituals. Your role is to be their coach and cheerleader, encouraging them as they face their fears.
Prioritizing Your Own Well-being as a Supporter
You cannot pour from an empty cup. Supporting someone with OCD is emotionally taxing, making self-care for caregivers essential. Make time for your own hobbies and friendships, consider joining a support group for families, and don't be afraid to seek your own therapy if you feel overwhelmed. Your well-being is not selfish; it's necessary.
Encouraging Professional Help: The Path to Recovery
While your support is invaluable, it is not a substitute for professional treatment. The ultimate goal is to guide your loved one toward evidence-based care. Encouraging professional help is often the most significant and impactful step you can take.
When and How to Suggest Seeking Therapy
Choose a calm, private moment to discuss therapy. Frame it as a sign of strength and a practical step toward feeling better, not as a judgment of their character. You could say, "I've noticed how much you've been struggling, and it hurts me to see you in pain. I've been reading about some really effective therapies for this, and I'll support you in any way I can if you're open to exploring them."
Understanding Effective OCD Treatments (e.g., CBT, ERP)
Educate yourself on the gold-standard OCD treatment options. Cognitive Behavioral Therapy (CBT), specifically a method called Exposure and Response Prevention (ERP), is the most effective treatment for OCD. In ERP, individuals gradually confront their fears (exposure) without engaging in compulsions (response prevention), helping them learn that their anxiety will decrease on its own.

Taking the First Step: Our Confidential OCD Test
Suggesting therapy can feel daunting. A gentle, non-threatening first step can be incredibly helpful. Encouraging your loved one to take a free OCD test provides a private, confidential way for them to explore their symptoms and see how they align with common patterns of OCD. It can be the catalyst that validates their experience and motivates them to seek a professional diagnosis.
Supporting a loved one with OCD is a journey of understanding, patience, and compassion. By educating yourself, practicing effective communication, setting healthy boundaries, and encouraging professional help, you can make a profound positive impact on their recovery. Remember, you don't have to navigate this alone, and your support matters more than you know.
For an initial, confidential insight into potential OCD symptoms, you or your loved one can start your self-assessment today. It's a safe, private first step towards gaining clarity and finding the right path to effective support and recovery.
Frequently Asked Questions for Supporters of Individuals with OCD
What should you NOT say to someone with OCD?
Avoid minimizing their feelings with phrases like "Just relax" or "Don't worry." Also, refrain from participating in rituals or offering reassurance, as this can strengthen the OCD cycle. Focus on validating their emotions without validating the obsessive fear.
How can I tell if my loved one might have OCD?
Look for a pattern of distressing, intrusive thoughts (obsessions) followed by repetitive behaviors or mental acts (compulsions) that take up a significant amount of time—often more than an hour a day—and cause notable distress or impairment in their life. A great starting point is to explore the symptoms with a confidential online tool.
Can a person with OCD live a normal and fulfilling life?
Absolutely. With the right evidence-based treatment, like ERP therapy, and a strong support system, individuals with OCD can effectively manage their symptoms and lead full, happy, and productive lives. Recovery is not just possible; it's expected.
What are common triggers for OCD symptoms that I should be aware of?
Triggers are highly individual but often include stress, fatigue, major life changes, or situations that directly relate to their specific obsessions (e.g., a public restroom for someone with contamination fears). Helping your loved one manage their overall stress can reduce the intensity of their symptoms.
Is it my fault if I accidentally enable their compulsions?
No. It's a natural human instinct to want to comfort someone you love. Many family members fall into the pattern of accommodating rituals without realizing it's unhelpful. The important thing isn't past behavior but your willingness to learn and change your approach going forward. Be kind to yourself as you learn.